Compliantly Optimize Healthcare Reimbursements
Denials and underpayments are defects in the revenue cycle that indicate a provider’s inability to comply with payer requirements or a payer’s inability to accurately pay a claim. CRN Healthcare Solutions works with practices to evaluate and implement lean process workflow denials management so that every dollar not paid which should have been paid is addressed and followed up.
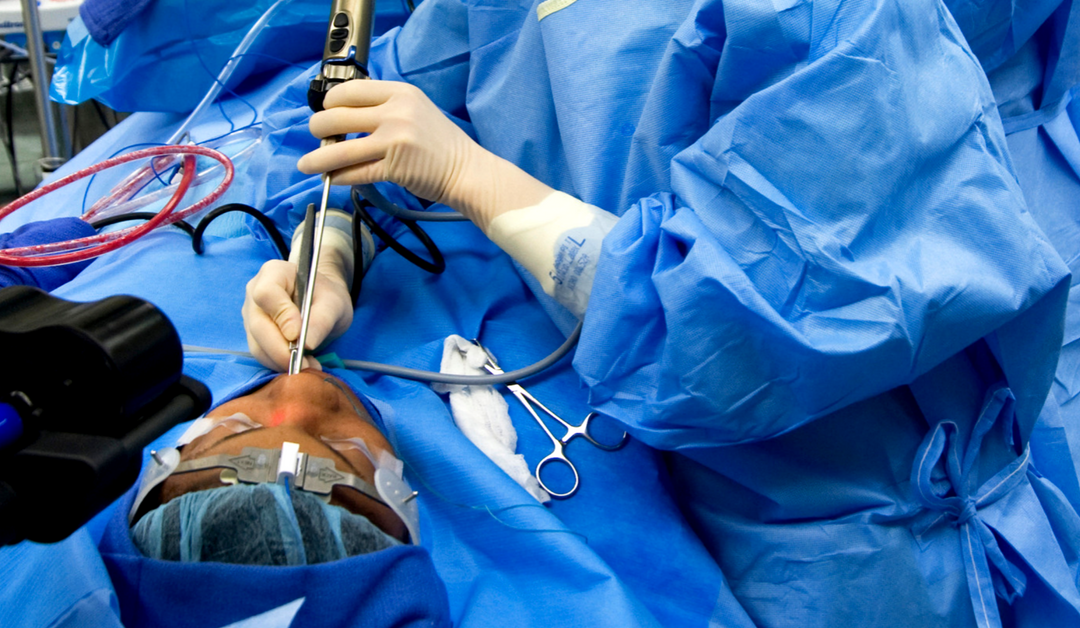
CMS Proposes Payment Changes to Endoscopic Sinus Codes
The Centers for Medicare & Medicaid Services (CMS) is proposing major payment changes to sinus endoscopy services. The 2020 Physician Fee Schedule (PFS) proposed rule includes the following excerpt: We are proposing to apply the special rule for m… For more,...

Anthem Changes Timely-Filing Deadlines
Anthem has sent out a notice to all providers who have signed non-Medicare or Medicare Advantage contracts with them, stating: “Effective for all commercial and Medicare Advantage Professional Claims submitted to the plan on or after Oct. 1, … For more, read...

ICD-10 Guidelines: Sometimes You Have to Break the Rules
Rik Salomon, CPC, CRC, CEDC, CEMA, CMCS, and I recently got into a rather spirited debate with a group of Certified Professional Coders (CPCs®) on coding guidelines and how they govern our medical coding. CPT® and ICD-10 guidelines are the primary det… For more,...

Reporting Bilateral Services: Conflicting Information Causes Confusion
Payer-specific rules — especially rules that vary for every claim — not only make collecting revenue difficult, but also add to the cost of collection of monies earned by the physicians. A blog clarifies Novitas’ instructions for reporting modifier … For more,...





